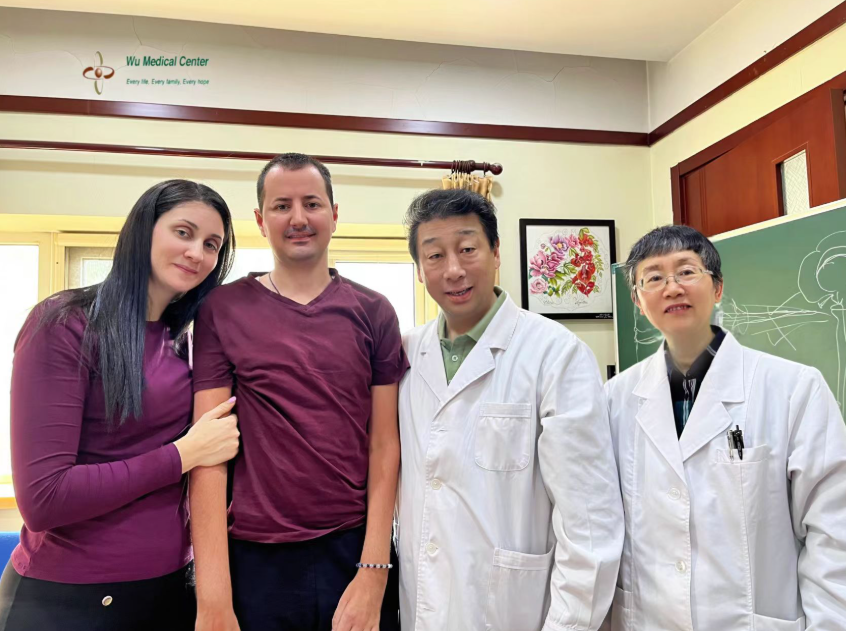
Nikola Mihajlović-Amyotrophic Lateral Sclerosis (ALS)-(Serbia)
 Patient Name: Nikola Mihajlović
Patient Name: Nikola Mihajlović
Gender: Male
Age: 34 years old
Nationality: Serbia
Diagnosis: Amyotrophic Lateral Sclerosis (ALS)
Condition upon Admission:
The patient had experienced progressive weakness in all four limbs accompanied by moderate muscle atrophy for over three years. He had had difficulty speaking for one year, with a weak voice and unclear articulation. His respiratory function was mildly reduced. In the last six months, he had experienced multiple episodes of fainting.
Physical Examination upon Admission:
The patient had a heart rate of 50-60 beats per minute, a respiratory rate of 22 breaths per minute, blood pressure of 128/84 mmHg, and oxygen saturation of 94-95%. He was thin in appearance. Both conjunctivae were chronically congested, with increased tear flow. There was no cyanosis of the lips, and the pharynx showed no congestion. His thorax was symmetrical, with reduced respiratory movement, and no significant dry or moist rales were heard. Heart sounds were strong, with a slow and regular rhythm, and no murmurs were detected in any of the cardiac valve areas. His abdomen was soft and flat, with the liver and spleen not palpable below the costal margin.
Neurological Examination:
The patient was alert but had a fair mental state. His speech was weak and articulation was unclear. His memory and calculation abilities were normal. Both pupils were 3 mm in diameter, with a brisk light reflex, and eye movements in all directions were normal. The nasolabial folds and forehead wrinkles were symmetrical. Tongue protrusion strength was weak (only just clearing the lips), with atrophy and fasciculations of the tongue muscles, and tongue movement was slow. His chewing strength was weak. The elevation strength of both soft palates was acceptable, and the uvula was centrally positioned. Neck rotation and shoulder shrug strength were grade 4. Muscle strength in the left upper limb was grade 2, the right upper limb was grade 2-, grip strength in the left hand was grade 2, and in the right hand, thumb strength was grade 0, while the strength of the other four fingers was grade 2-. Muscle strength in the left lower limb was grade 3 and in the right lower limb was grade 3-. In the supine position, the left hand could be raised to the mandible, and the right hand could be raised to the chest. The patient was unable to lift both upper arms off the bed against gravity. His left wrist demonstrated dorsiflexion but not against resistance; he could flex and extend all five fingers and grasp, although with poor resistance. The right wrist showed weakness and presents in a wrist drop position, with no functional movement of the right thumb, while the other four fingers could slowly flex and extend and grasp, again with no resistance. Muscle strength in both lower limbs was diminished; in the supine position, he could bend both legs and lift them off the bed, with the left leg raised approximately 15 cm and the right leg about 10 cm, but he could only maintain this for about 5 seconds. The left ankle could perform dorsiflexion and plantarflexion, whereas the right ankle could not. He was unable to stand independently. Muscle atrophy was present in all four limbs, with visible fasciculations. Muscle tone in both upper limbs was mildly increased, while tone in both lower limbs was significantly increased. Both superficial and deep sensations were normal. Tendon reflexes were present in both upper limbs, but were hyperactive in both lower limbs. The Hoffmann and Babinski signs were positive bilaterally. His hand alternating test was slow, and he was unable to complete the finger-to-nose test or the finger-to-finger test due to inadequate strength. The performance of the heel-knee-shin test was poor on both sides. Meningeal signs were negative.
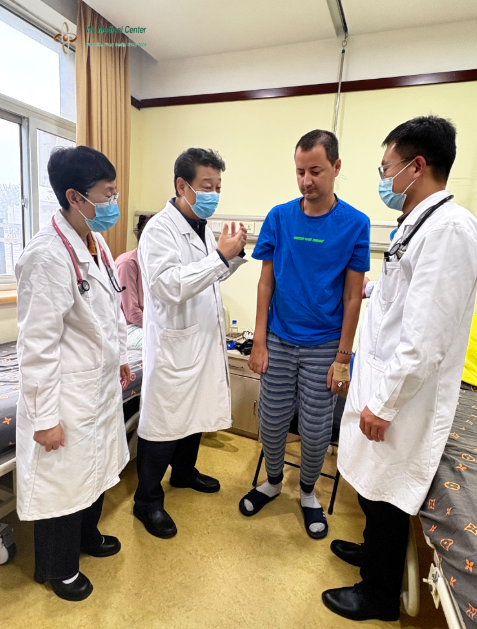
Treatment Process:
The patient was diagnosed upon admission with "Amyotrophic Lateral Sclerosis (ALS)." During the hospitalization, he received treatment aimed at repairing motor neuron damage using neural stem cells. Additionally, mesenchymal stem cells were administered to provide neurotrophic, endocrine, and immune support. The treatment regimen included the adjunctive use of edaravone, riluzole, neurotrophic factors, reduced glutathione, and human immunoglobulin as part of the CAST treatment approach. Comprehensive rehabilitation therapy was also integrated into his treatment plan to support functional recovery and improve quality of life.
Post-Treatment Assessment:
The patient exhibits significant improvement in motor function, with an overall enhancement of approximately 30%. Respiratory function is improved, with blood oxygen saturation levels ranging from 96% to 98%. He reports an increase in speech volume, with more coherence and fewer pauses. Cardiac function is stabilized, maintaining a heart rate above 60 beats per minute. Incidents of syncope has largely resolved. Muscle strength assessment shows the following: Left upper limb strength is improved to grade 3, and right upper limb strength to grade 3-. In the supine position, both upper arms can be raised 10 cm off the bed against gravity, and in a seated position, he can lift both hands to chest level while overcoming gravity. Grip strength is increased to grade3+ in the left hand and grade 3- in the right hand, allowing him to grasp another person's fingers and resist a degree of force. In the lower limbs, muscle strength is improved to grade 4-, with both legs able to lift approximately 30 cm off the bed; the left leg can hold this position for about 15 seconds, while the right leg can maintain it for 8-10 seconds. He achieves the ability to stand independently and can begin walking with assistance. Overall, his physical stamina and exercise tolerance shows improvement. Additionally, conjunctival hyperemia is resolved, and the excessive tearing has largely subsided.